CodeValidate
CodeValidate enables searching for Medical Necessity issues and CCI edits in a single entry panel. CodeValidate includes the following modules:
- Billable Units Calculator
- MS-DRG Grouper
- OPPS Calculator Outlier Payments
- VitalABN (Advanced Beneficiary Notice)
Accessing CodeValidate
To access CodeValidate, select Products > VitalKnowledge > CodeValidate.
Claim Input Validation Walkthrough
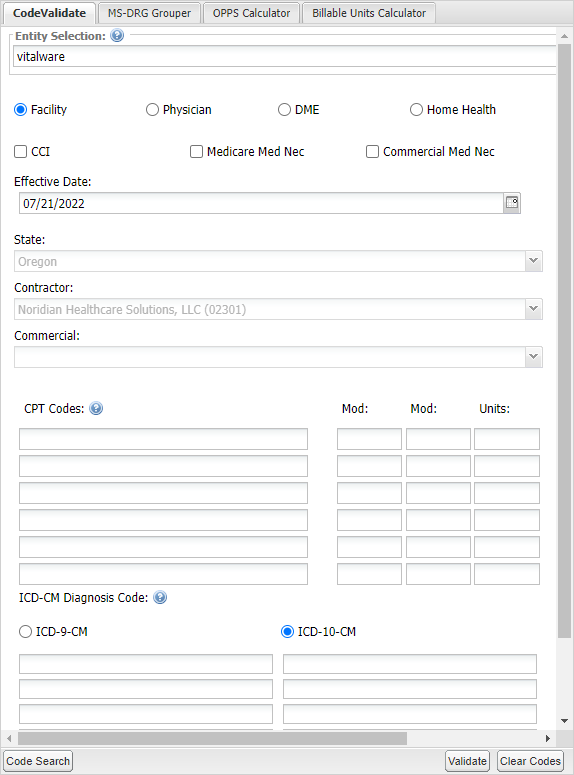
The Claim Input panel on the left defaults to your primary entity, state and contractor.
- Choose the type of bill you are validating: Facility, Physician, DME, or Home Health.
- Choose CCI, Medicare Med Nec, Commercial Med Nec, or a combination to validate.
- Aetna
- Anthem
- BCBS Alabama
- BCBS Empire
- BCBS Excellus
- BCBS Illinois
- BCBS Massachusetts
- BCBS Mississippi
- BCBS Montana
- BCBS New Mexico
- BCBS Oklahoma
- BCBS Rhode Island
- BCBS Texas
- BCBS Wyoming
- CA Medi-Cal
- Capital BCBS
- Cigna
- ConnectiCare
- Highmark BC PA
- Highmark BCBS of Delaware
- Horizon BCBS of New Jersey
- Humana
- Husky Health
- Independence BCBS
- MassHealth
- NH Healthy Families
- Regence
- UnitedHealthcare
- Change the Effective Date to the claim date of service.
- If necessary, change the State. The appropriate contractor will be assigned using the type of bill and state selected.
- Enter the CPT codes on the claim. If you have more than the default six, more fields will populate as you input codes.
- Enter the Modifiers assigned to each code.
- Enter the number of Units to check for MUE issues.
- Enter the ICD-10 Diagnosis codes on the claim. Capitalization and decimal points are not necessary.
- Click Validate to populate results.
- If you need to look up a code to add to the validation, click Code Search in the bottom left corner to open Code Lookup.
- After you search and find the code you want to add, select it and click Add Selected at the bottom of the window, then click close.
Note: If you select Commercial Med Nec, the following payers are available:
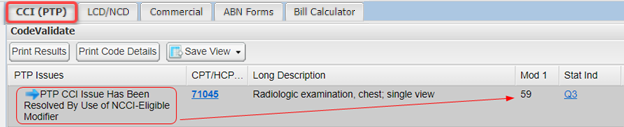
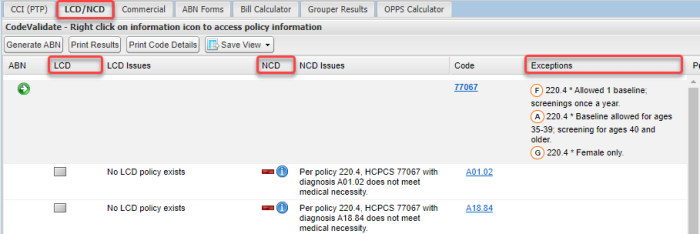
CCI and LCD/NCD results will appear on separate tabs to the right of the CodeValidate panel.
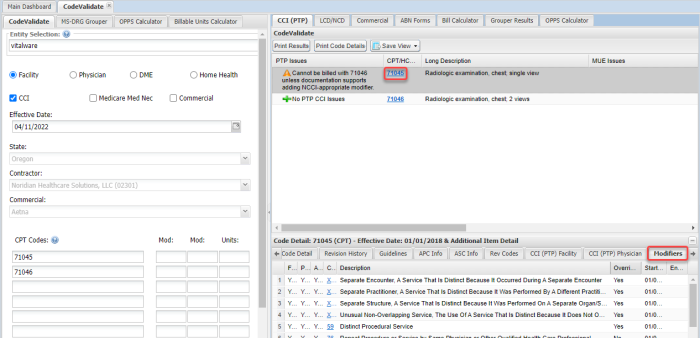
The CCI tab provides information on any CCI issues found based on the CPT/HCPCS codes you entered. It will also validate that the Modifiers used are best practice and will alleviate the CCI issues.
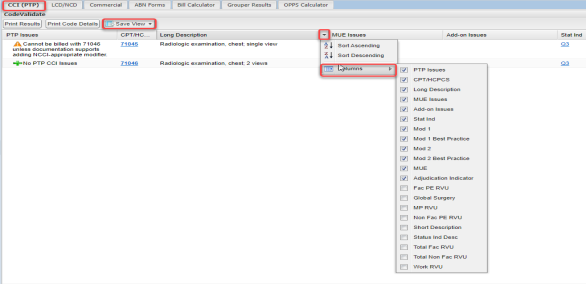
Customize the columns you would like in your view by clicking any column header. Select the columns you want to see, drag the columns into the order you prefer, and then click Save View.
Click any blue CPT code to open the Modifiers tab of the Code Details panel at the bottom of your screen.
The LCD/NCD tab provides information on Local and National Coverage Determinations found based on the CPT and Diagnosis codes you entered.
The Exceptions column displays any age, gender, or frequency limitations on a code.
Right-click any  icon to access a hyperlink that opens the entire policy in a new tab.
icon to access a hyperlink that opens the entire policy in a new tab.